Episode 054: Breast Cancer Series, Pt. 3-Breast Cancer Vocabulary
The language of breast cancer can be confusing and very technical. In this episode, we help you learn and understand so many important words and phrases that have important implications on diagnosis and management. Understanding these will not only help you learn more about breast cancer, but it will also ensure you are better able to communicate the lingo to your patients!
First we start out with a breakdown of the important terms you may see on a pathology report about a patient’s diagnosis.
How do we classify breast cancer:
Hormone receptor status by immunohistochemistry (IHC): As discussed in episode 003, IHC helps detects the phenotype of the cell
Estrogen receptor (ER+)
Presence predicts response to estrogen blocking agents
Cut off is >= 1% of the cells are positive
Progesterone receptor (PR+)
Often ER/PR+ can be called “Hormone receptor positive”
You CAN have ER+ without PR+
HER2 status by IHC and/or Fluorescence in situ hybridization (FISH):
IHC:
(Infographic by Ronak Mistry)
FISH: using colored probes (also covered in Episode 003)
HER2 locus is on chromosome 17
Green probe = control = CEP17 which is centromere 17
Red probe = HER2 gene
Lots of red and little green = HER2 amplified
Remember 2, 4, 6
HER2 signal >6 = positive
Ratio of HER2/CEP17 >2 and HER2 >4= positive
HER2 >/= 4 but <6 and/or HER2/CEP17 ratio <2.0 → equivocal
They re-assess/ask another pathologist to look at the slides
If still equivocal, then considered HER2 negative with a comment
HER2 <4 signals/cell and/or HER2/CEP17 ratio <2.0 → negative
Morphologically:
Based on anatomy of the breast
Invasive vs. in situ:
Did tumor break through the duct and into the adjacent issue?
Lobular carcinoma in situ:
Lobules are milk-producing glands
LOCALIZED cancer in the lobule
Not considered to be a precursor to cancer, but does suggest patient is high risk
Ductal carcinoma in situ:
Ducts carry milk from the lobules
LOCALIZED cancer in the ducts
Considered to be precancerous to invasive cancer
If not in situ then we typically see invasive ductal but could see alternative histologies
May see terms like invasive mammary carcinoma or invasive breast cancer “no special type” - which is synonymous with invasive ductal carcinoma which is going to be the most common type of breast cancer
This is in contrast to the other histologic subtypes called “special types”
These can portend a better prognosis if they are a pure special type histology with a few exceptions (note can have mixed picture with some special type histologic features)
Data is very limited so hard to draw significant conclusions
Largest study comes from Korean Breast Cancer Registry:
Lobular
Mucinous (also called colloid breast cancer)
Micropapillary = often higher grade with more LVI
Metaplastic = often TNBC with worse prognosis in general compared to NST
Special type of tumor = malignant phyllodes tumor
Think of this like a soft tissue sarcoma
Need good surgical excision
Grade:
Grade 1, 2, and 3
Just remember 3 is worst prognosis (high grade) and 1 and 2 are often lumped together (low to intermediate grade)
Three components of a score to determine grade:
Tubule formation (more tubules = normal growth = lower grade)
Nuclear pleomorphism → large and weird nuclei = higher grade
Mitotic count
Ki67:
Can be thought of as a measure of how fast cells are growing
Has clinical utility only for prognosis in patients with ER+/HER2- patients who don’t need chemotherapy
Important to note given its implications on the use of targeted agent known as abemaciclib
Lymphovascular invasion:
The presence of tumor invading lymph nodes and blood vessels, which in general suggests higher risk features and can affect radiation planning
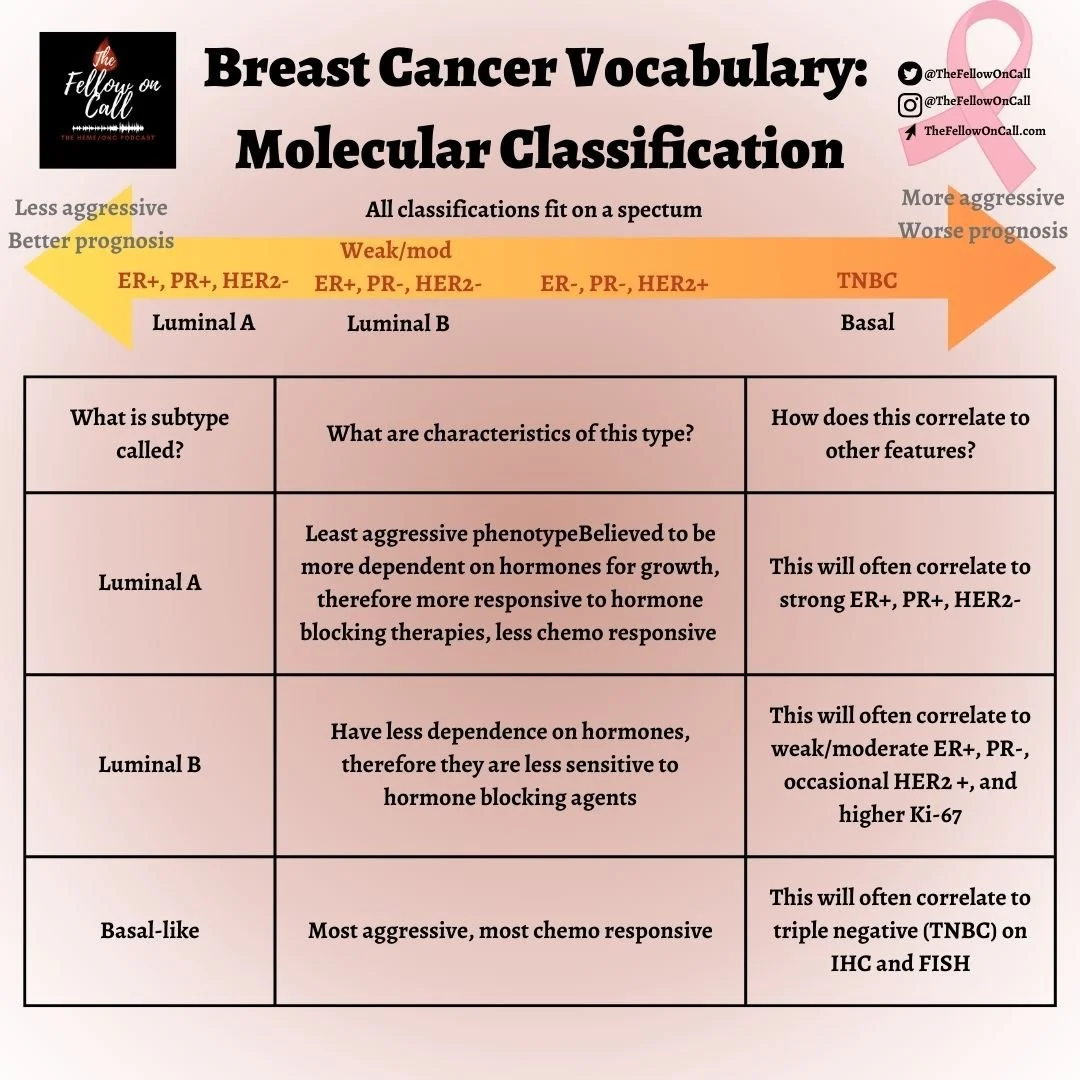
Molecular Classification of Breast Cancer
Historical Context
Several individual studies showed that women with ER positive tumors had a lower response to chemotherapy than ER negative tumors
Thought was that we might be overtreating women with chemotherapy so we needed more than just IHC and FISH
Original publication by Perou and colleagues in 2000 showed six different molecular subtypes could be predictive of response to chemotherapy and prognostic for recurrence
Subtypes defined based on multi-gene assays often look at those associated with ER signaling → note this is not done routinely as we still use IHC and FISH to guide treatment
Three common molecular subtypes to be aware of:
(Infographic by Ronak Mistry)
Also had HER2-enriched, claudin-low, and normal breast-like
Molecular understanding of cancers lead to development of assays used to determine if patients with ER+ breast cancer need chemotherapy:
Most common that we have are “Oncotype Dx” (21 gene assay) and “Mammaprint” (70 gene assay)
These provide a score that lets us understand both the prognostic recurrence risk and now have been validated as predictive tools to guide chemotherapy decisions
Specific Molecular testing (often done via NGS):
Looking for mutations that provide targets
ESR1 mutation is important → dictates switch of endocrine therapy from AI to a SERD
PIK3A mutation is important → targeted pill therapy
Important surgical terminology:
Lumpectomy aka breast conservation surgery aka partial mastectomy: Only the mass and some surrounding tissue is removed
Mastectomy: Whole breast is removed
Margins:
When performing lumpectomy, the surgeon will use ink to draw a circle around the tumor + some adjacent healthy tissue. When the pathologist looks at the tissue under microscope, we are hoping to see “no ink on tumor” meaning that there is healthy issue surrounding the tumor that has been removed.
If there is tumor at the ink line, double risk of recurrence
Clear margins has the lowest chance of recurrence
For invasive cancer: Society of Surgical Oncology and American Society for Radiation Oncology recommend “no ink on tumor” based on results of a large met-analysis. Essentially, they are saying that wider margins (for instance >2mm) is no different in terms of outcomes than narrower margins
For DCIS: SSO and ASTRO recommend 2mm margins also based on meta-analyss
General approach to TNM staging
Think about it as dollar bill amounts → similar to the mnemonic for the common pathway of the coagulation cascade
Think 1 dollar, 2 dollar (don’t forget we used to have the 2 dollar bill), and 5 dollar bill
T1C = > 1 cm
T2 = > 2 cm
T3 = > 5 cm
Nodal disease → the axilla is key
Mobile axillary nodes palpable = N1
Fixed or matted axillary nodes palpable = N2
Internal mammary nodes (IMN) without axillary nodes = N2 → think inner quadrant of breast → N2 because these are central nodes
Everything else = N3
Endpoint descriptions for non metastatic trials:
Often use surrogates for OS which have not been definitely validated
DFS = Disease free survival
Got definitive treatment surgery +/- radiation +/- systemic therapy
Time until recurrence of cancer in either breast, distant disease, second cancer, or death
Second cancer is important as we are giving chemo that could cause MDS and leukemia which should be considered when giving to a large population
iDFS = Invasive Disease Free Survival
Same except DCIS does not count
RFS = Recurrence free survival
Same as disease free survival without second cancer counting
EFS = time to progression of disease
This is used commonly in neoadjuvant trials
Pathologic CR
This is also commonly used in neoadjuvant trials
References:
https://link.springer.com/article/10.1007/s10549-020-05861-6: Korean Breast Cancer Registry about different tumor subtypes
BreastCancerNow.org: Great resource for general information for patients about breast cancer
https://www.nature.com/articles/35021093: Molecular subtypes of breast cancer
https://www.breastcancer.org/research-news/20140402: Article about tumor margins
https://www.uptodate.com/contents/breast-conserving-therapy?search=breast%20cancer%20margins&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H15 : Article about tumor margins
The crew behind the magic:
Show outline: Ronak Mistry, Vivek Patel
Production and hosts: Ronak Mistry, Vivek Patel, Dan Hausrath
Editing: Resonate Recordings
Shownotes: Ronak Mistry
Graphics, social media management: Ronak Mistry