Episode 105: Colorectal Cancer Series, Pt. 7 - Management of Rectal Cancer
This week, we incorporate medical oncology back into our discussion with our Radiation Oncologist, Dr. Sanford, and our Surgical Oncologist, Dr. Bailey. We discuss how we approach the management of localized rectal cancer. Note that we will be heavily building off our discussions with our specialist. We recommend listening to these episodes if you have not done so already.
What important information do we need to be aware of when approaching a patient with rectal cancer?
Rectal cancer is defined as tumor up to 15 cm from the anal verge
Low: 1-5 cm from anal verge
Mid: 5-10 cm from the anal verge
Upper: 11-15 from the anal verge
Need to know microsatellite stability/mismatch repair status. This has implications on treatment options
Need CT and pelvic MRI imaging. This has implications on staging and also how we determine neoadjuvant therapy.
What we can learn from MRI:
T stage of the rectal tumor
If T4 then needs neoadjuvant chemoradiation and chemotherapy and can’t go straight to surgery
Distance from the anal verge and presence of sphincter involvement
If within 5 mm of the anal verge, the tumor is considered low lying and these patients often have sphincter involvement requiring an APR as we discussed in our surgical episode
Low lying tumors often require neoadjuvant chemoradiation and chemotherapy in hopes to allow for sphincter preservation and organ preservation in some cases
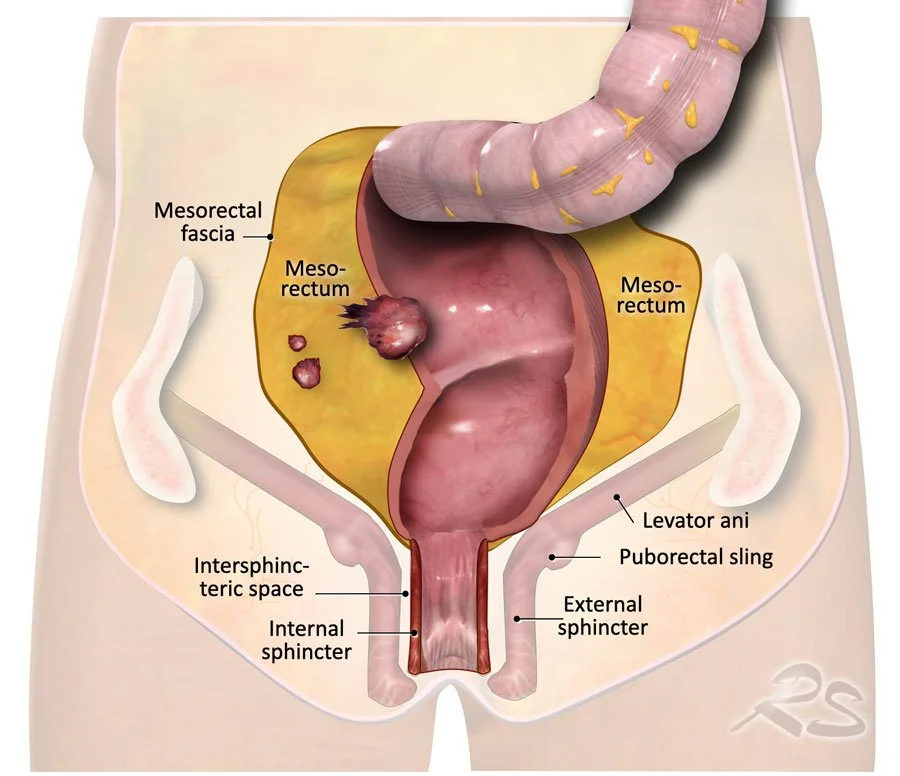
Involvement of the mesorectal fascia or sometimes referred to as threatened circumferential resection margin
If the tumor is within 1 mm of the mesorectal fascia, this is a prognostic factor for locoregional recurrence, therefore treating with neoadjuvant chemoradiation and chemotherapy prior to surgery would be recommended
Extramural venous invasion
High risk feature for distant recurrence that requires neoadjuvant chemoradiation and chemotherapy therapy
Lateral pelvic lymph node involvement
High risk and requires neoadjuvant chemoradiation and chemotherapy
Source: https://www.cancer.org/cancer/types/anal-cancer/about/what-is-anal-cancer.html. No copyright infringement intended.
How did we arrive at the use of neoadjuvant radiation therapy and surgery with total mesorectal excision?
In 1990s, there were several studies looking at the incorporation of 5-FU in the adjuvant setting for both colon and rectal cancer
For rectal cancer, there were implications on quality of life and permanent ostomy after surgery, therefore there was a push to do two things:
Make surgical technique better
Incorporate radiation for better local control in hopes that this also translates to better distant disease recurrence rates
The first major breakthrough was development of the “total mesorectal excision” (TME)
We discuss this in our surgical episode, but briefly, this is removing the fat surrounding the rectum which contains a majority of the locoregional lymph nodes
Improvements in radiation were also studied, which we also discussed in our Radiation Oncology episode:
In Europe, “short course radiation,” which was 5Gy delivered in 5 fractions was the standard based on the Swedish Rectal Cancer Trial in 1997
A flaw of this study was that TME was not required; a follow up study called the Dutch Colorectal Cancer Group TME trial solidified the efficacy of short course radiation before TME showing the same locoregional recurrence and OS benefit
In the United States, there was more enthusiasm for “long course hypofractioned concurrent chemoradiation therapy” delivered over 5 weeks given significant benefit in older studies in the adjuvant setting
There were three studies that established improved locoregional recurrence and higher rates of sphincter preservation with preoperative long course chemoradiation compared to postoperative chemoradiation
This is why you will see long course chemoradiation used in some trials and short course radiation used in other trials.
Be sure to check out our radiation oncology episode where we talk more about the nuances
Note: We do NOT have data to suggest that one is better than the other!
Image source: https://radiologyassistant.nl/abdomen/rectum/rectal-cancer-mr-staging-1. No copyright infringement intended.
Where did we derive the high risk factors from?
There were several analyses looking at prognostic factors in locoregional and distant recurrence in rectal cancer which is where those high risk features originally came from
How did we arrive on the impact of neoadjuvant therapy?
There were a few trials that tried to determine if long course vs. short course radiation was better; there was no difference.
One of these trials was the Stockholm III Study:
Study design: Non-inferiority randomized trial which randomized patients with resectable rectal cancer to:
Short course radiotherapy (5 fractions x 5 days) followed by surgery within 1 week
Short course radiation followed by surgery within 4-8 weeks to allow
Long course chemoradiation over 5 weeks followed by surgery in 4-8 weeks
Roughly 20% of patients received adjuvant chemotherapy
Outcomes: No difference in locoregional recurrence, distant metastasis, or overall survival
It did show that there was more pathologic tumor downstaging when delaying 4-8 weeks after short course radiation which makes sense because you are giving more time for radiation effects to kick in
This trial, among others, is why European countries still often prefer short course radiotherapy as opposed to long course chemoradiation
Since there was no major difference between long vs. short course, the field started incorporating chemotherapy with either short course radiation or long course chemoradiation prior to surgery
Focused this on patients with high risk disease to improve pathologic complete response
Essentially, this was throwing the kitchen sink at patients; This became known as “Total Neoadjuvant Therapy” or TNT
In our radiation oncology episode, we mentioned the RAPIDO trial. Let’s go through this trial.
Based on the results of the Stockholm III study which suggested that delaying surgery after short course radiation was beneficial before surgery, the thought was that this provided a window of opportunity to incorporate chemotherapy preoperatively to prevent distant metastases without compromising locoregional disease control
The RAPIDO Trial (“Rectal Cancer and Preoperative Induction Therapy followed by Dedicated Operation”) included patients from USA and Europe with locally advanced rectal cancer that was considered high risk by one of the following MRI findings:
T4 or N2
Extramural vascular invasion
Involved mesorectal fascia
Enlarged lateral pelvic nodes
Patients were randomized to either:
Preoperative long course chemoradiation followed by surgery followed by optional adjuvant chemotherapy x 24 weeks per the discretion of the local hospital
The TNT approach: Short course radiation followed by 18 weeks of chemotherapy followed by surgery
The primary endpoint was disease related treatment failure which was a composite endpoint of locoregional failure, distant metastasis, new primary colorectal tumor, or treatment-related death
In the initial publication in 2021:
There was a statistically significant improved disease related treatment failure rate favoring the TNT approach by about 7% (23% vs. 30%)
There were similar rates of locoregional control but path CR was higher in TNT at 28% compared to 14% → so double the percentage of path CR
There was a lower rate of distant metastasis favoring the TNT approach by about 7% (20% vs. 28%)
In the 5 year follow up publication in 2023:
There was worse locoregional failure rates in the TNT approach compared to preoperative long course chemoradiation (10% vs. 6%)
There was still improved distant metastasis rate favoring the TNT approach
This really told us that TNT has high path CR rates but there is still possibly worse locoregional failure with the use of short course radiotherapy as opposed to long course chemoradiation
Hmm… are there flaws in this study that we should be aware of that could have lead to these results?
Unfortunately, we don’t have a direct comparison of TNT with short course radiation vs. long course chemoradiation from this trial
All patients get chemotherapy in the TNT arm while on 40% of patients got adjuvant chemotherapy in the preoperative long course chemoradiation arm which can explain the difference in distant metastatic disease favoring TNT
This is a reminder that path CR is not a perfect surrogate endpoint in cancer clinical trials
There was also no difference in overall survival or quality of life metrics at 3 years
This might make you advocate for the use of long course chemoradiation for all patients in the TNT setting, but there is a counter argument to be made
More of the patients in the TNT arm got LAR instead of an APR which makes you wonder if surgeons chose a sphincter preservation given view of tumor downstaging and actually left behind tumor deposits
The trial was not powered for a difference in locoregional failure so the effect size may not be as large as we think
Time may have been a factor with 40 weeks of treatment time prior to TNT compared to 25 weeks in the long course chemoradiation group
Instead of looking at long course vs. short course, maybe we need to meet somewhere in the middle to optimize local control and prevent distant metastatic disease
Last year, in our post-ASCO collaboration series, we discussed the PROSPECT trial which was presented at the plenary session. What did that trial show and who might benefit from omission of preoperative radiation?
This was a really important study and validates the idea that refining patient selection is key as we give TNT to more patients
NOTE: When this study was designed, remember that there was not widespread use of TNT for patients with rectal cancer and preoperative long course chemoradiation was standard in the United States
Study design:
Patients with T2-T3 mid to upper rectal cancer without high risk MRI features were randomized to:
Preoperative FOLFOX x 3 months followed by sphincter preserving surgery
In order to omit radiation in the chemotherapy only arm, the tumor had to decrease in size by at least 20% on repeat imaging to proceed to surgery and otherwise patients would be salvaged with chemoradiation
Preoperative long course chemoradiation followed by sphincter preserving surgery
Adjuvant chemotherapy was optional in both arms
Outcome: There was no difference in DFS or OS between the groups
This really told us that omission of preoperative radiotherapy is reasonable in select patients
We learned some important patient reported outcomes from this study:
During neoadjuvant treatment, side effect profile favors the chemoradiation group
At 12 months after treatment, there was improved neuropathy, fatigue, and sexual function favoring the chemotherapy only group
There was no difference in bladder symptoms
This is important to consider for younger patients and shared decision making is important in these earlier stage tumors
Is there data for non-operative management in rectal cancer?
The best data for this is from the Organ Preservation in Rectal Adenocarcinoma (“OPRA”) Trial
These patients did NOT have MSI-high disease
Study design:
Phase II study
Patients who did NOT have MSI-high disease were randomized patients to either long course chemoradiation followed by chemotherapy x 16 weeks vs. chemotherapy x 16 weeks followed by long course chemoradiation
Basically induction chemoradiation followed by chemo vs. induction chemo followed by chemoradiation
Included patients with Stage II and Stage III rectal adenocarcinoma with 70% of patients enrolled having lymph node involvement
About 50% of patients did not need surgery at 5 year follow up for patients who got chemoradiation first followed by chemotherapy
This was better than chemotherapy first where 40% of patients did not need surgery at 5 year follow up
Patients who are eligible and opt for this route require a lot of monitoring, as we discussed in our surgery episode, including flexible sigmoidoscopy and MRI every 4 month x 2 years and then every 6 months x 3 years. Therefore, patients need to be aware of this commitment.
Is there any data for treatment of rectal cancer without either radiation or surgery?
In 2022, there was a NEJM article of a single center phase II study that included stage II and III patients with rectal cancer and MSI-high tumors
There were 12 patients enrolled and given the anti PD1 antibody dostarlimab q3week x 6 months
There was a 100% complete clinical response rate and no patients proceeded to chemoradiation or surgery
This was an incredible breakthrough for patients and use of immunotherapy for non operative management in MSI-high patients is standard of care
References:
https://www.nejm.org/doi/full/10.1056/NEJM199704033361402: Swedish Rectal Cancer Trial providing data for short course radiation
https://www.sciencedirect.com/science/article/pii/S1470204511700973?via%3Dihub: Dutch Colorectal Cancer Group TME Trial providing data for short course radiation in the TME era
https://ascopubs.org/doi/10.1200/JCO.2006.06.7629: Study providing data for long course chemoradiation
https://www.nejm.org/doi/full/10.1056/NEJMoa040694: Study providing data for long course chemoradiation
https://ascopubs.org/doi/10.1200/JCO.2009.22.0467 : Study providing data for long course chemoradiation
https://www.sciencedirect.com/science/article/pii/S1470204517300864?via%3Dihub : Stockholm III Study showing that waiting 4-8 weeks after radiation was better
https://www.sciencedirect.com/science/article/pii/S1470204520305556#sec1: RAPIDO Trial evaluating role of chemotherapy preoperatively
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10481913/: 5-year follow up on RAPIDO Trial
https://www.nejm.org/doi/full/10.1056/NEJMoa2303269 : PROSPECT Trial providing data for elimination of preoperative radiotherapy in a select population of patients
https://pubmed.ncbi.nlm.nih.gov/37270691/ : Patient reported outcomes from PROSPECT Trial
https://pubmed.ncbi.nlm.nih.gov/35483010/ : OPRA Trial evaluating non-operative management of rectal cancer
https://ascopubs.org/doi/10.1200/JCO.23.01208 : 5-year follow up data OPRA trial
https://www.nejm.org/doi/full/10.1056/NEJMoa2201445 : NEJM article on dostarlimab
The crew behind the magic:
Show outline: Vivek Patel
Production and hosts: Ronak Mistry, Vivek Patel, Dan Hausrath
Editing: Resonate Recordings
Shownotes: Ronak Mistry
Social media management: Ronak Mistry
We are proud to partner with HemOnc.org!
Want to learn more about the trials that lead to the regimens discussed today? What about dosing schedules? See links in the show notes for a link to HemOnc.org