Episode 103: Colorectal Cancer Series, Pt. 5 - Surgical Management of Colorectal Cancer
This week, we are joined by Dr. Christina Bailey, Associate Professor of Surgery and Program Director of the General Surgery Residency at Vanderbilt University Medical Center in Nashville, Tennessee, for a discussion about the role of surgery in the management of patients with colorectal cancer. This is another amazing multidisciplinary colorectal surgery episode you do not want to miss!
Rectal Cancer
Why is obtaining an MRI important for patients with rectal cancer?
Helps with clinical staging (T and N staging)
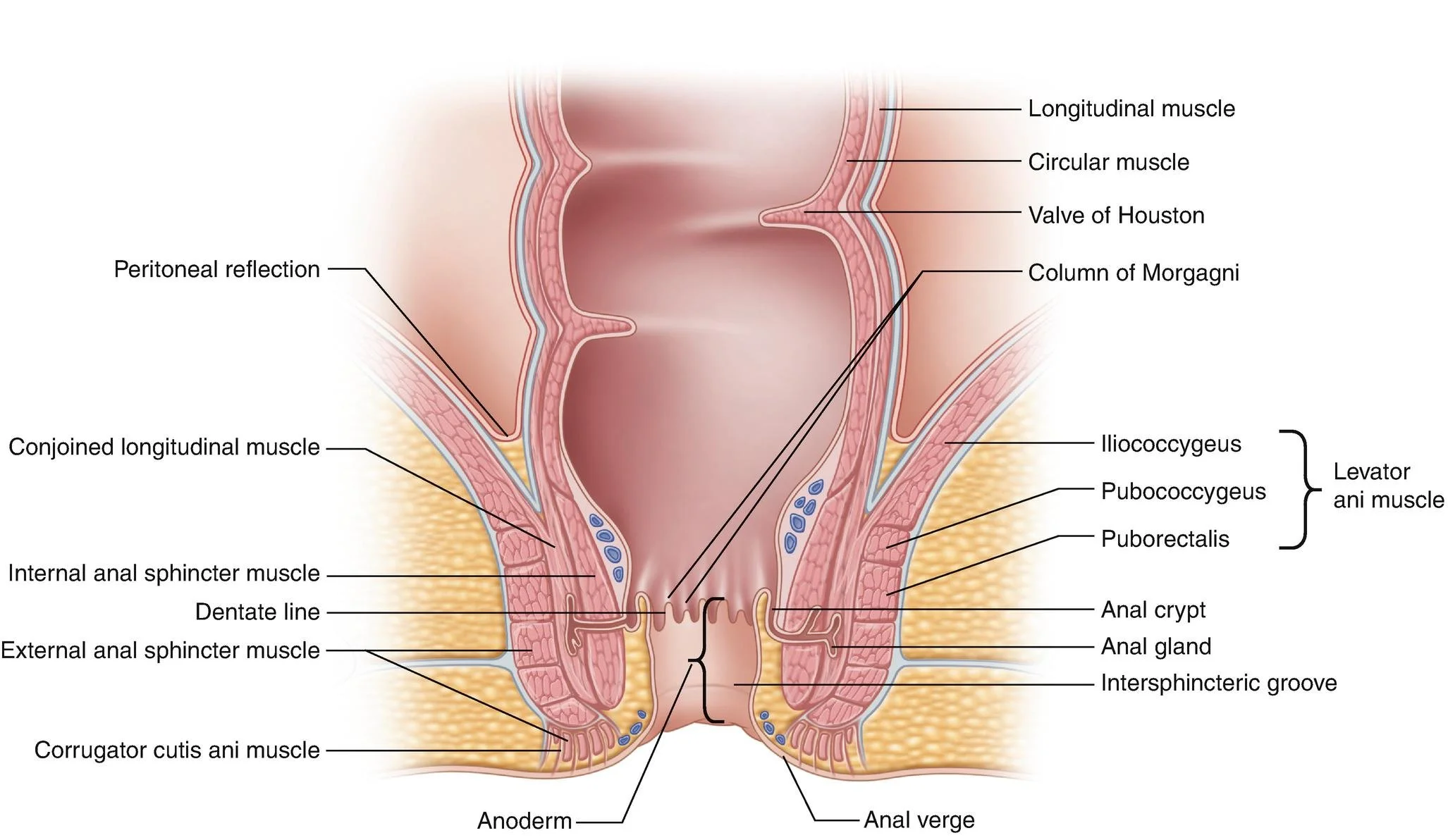
Also helps determine how far the tumor is from the anal verge and provides insight into if the sphincter is involved, which impacts the type of surgery that patients can have.
Image source: https://www.ascrsu.com/ascrs/view/ASCRS-Textbook-of-Colon-and-Rectal-Surgery/2285001/all/Anatomy_and_Embryology_of_the_Colon__Rectum__and_Anus (No copyright infringement intended)
What is the difference between an “APR” and an “LAR”?
LAR: low anterior resection
We are able to preserve bowel continuity
APR: abdominal perineal resection
This is a much more involved surgery most often necessary when the tumor involves the sphincter muscle
Rectal and anus are removed, resulting in permanent colostomy
How to decide between these two?
Location of the tumor is critical, with distal tumors being more amenable to LAR
However, this decision can be more complicated and more nuanced, particularly when tumors are close to but not involving the sphincter, requiring the surgeon to consider patient’s current physical status and bowel function
What are the long-term complications associated with these procedures?
Depending on how much of the rectum that needs to resected determines quality of life
LAR: Bowel habits will change; softer and more frequent bowel movements are more common (2-6 BMs per day)
APR: Colostomy in place, which will impact life
Many patients seen by surgery have undergone neoadjuvant chemoradiotherapy therefore they will also have side effects from that, including sexual dysfunction and urinary retention
What is total mesorectal excision?
The mesorectum is the fat around the rectum
So the surgeons are removing not only the colon but also following the planes of the fat around the rectum and removing this, too
Improves local recurrence rates
As a surgeon, what are your thoughts on non-operative management of rectal cancer, such as shown in the OPRA trial?
Great to improve outcomes and make positive impact on patient’s quality of life
Very important, though, that patients understand and adhere to a very stringent surveillance protocol for at least 2 years after completing therapy with regular surgery follow up, MRIs, and flex sigmoidoscopy
In patients who have recurrence of their rectal cancer after non-operative management who therefore require surgery, is the procedure more technically difficult because of the prior treatment with chemotherapy and radiation?
In Dr. Bailey’s experience there the procedures have not been more difficult and she has not noted more scar tissue from the prior radiation therapy
Colon cancer
When you see a new patient with colon cancer, how do you determine how much colon to remove?
How much colon to remove is dictated by the blood supply to the colon; she wants to remove the lymph nodes, which course with the blood supply. This also ensures that the adequate number of lymph nodes (at least 12) are removed.
How do you counsel patients on what to expect after surgery?
The biggest impact is going to be changes in bowel habits, with a slight increase expected.
Will typically not be as drastic as rectal cancer patients
In your experience, how often are less than 12 nodes removed?
This is rare at experienced centers, especially if following the blood supply
In the rare instances this happens, and many times there it is a sampling error. Re-evaluating the specimen often reveals that the adequate number of lymph nodes are present
How long after surgery do you advise patients to wait before starting adjuvant chemotherapy?
Depends on minimally invasive vs. open approach to surgery
MIS: 4-6 weeks
Open: 6-8 weeks
Which patients do you think would be good candidates for definitive local resection and treatment of metastatic disease?
She asks “can we remove the metastatic site and get negative margins,” while also factoring in patient’s functional status
Also want to consider tumor biology. In other words, if patients are responding to chemotherapy for the metastatic disease, these patients may benefit from surgery. Conversely, the tumors are not responding or new sites continue to arise despite chemotherapy, these patients are less likely to be good surgical candidates
About our Guest:
Dr. Christina Bailey is an Associate Professor of Surgery and Program Director of the General Surgery residency at Vanderbilt University Medical Center in Nashville, Tennessee. She has clinical interest in GI malignancies. Her research focuses on disparities in cancer diagnoses, treatment and outcomes in different ages, socioeconomic backgrounds, and race, as well as QOL outcomes in patients. Dr. Bailey completed medical school at Louisiana State University Shreveport, after which she completed her general surgery residency and chief residency Vanderbilt University Medical Center. She subsequently completed a fellowship in Complex General Surgical Oncology at MD Anderson Cancer Center prior to returning to Vanderbilt as faculty.
The crew behind the magic:
Show outline: Vivek Patel
Production and hosts: Ronak Mistry, Vivek Patel, Dan Hausrath
Editing: Resonate Recordings
Shownotes: Ronak Mistry
Social media management: Ronak Mistry