Episode 131: VTE Series-Approach to workup and initial management
This week, we kick off a new, highly-anticipated and highly-requested series, covering venous thromboembolism (VTE). In this first episode, we discuss how we make the initial diagnosis and how we approach initial management. As a clinician, you will undoubtedly come across the need to make this decision. This episode and this series will set you up for success!
This episode is sponsored by our Global Research Partners? Click here to get paid to participate in market research surveys!
What diagnoses fall under the umbrella of “venous thromboembolism?”
VTE as a category includes superficial venous thrombosis, deep vein thrombosis, and pulmonary embolism
When a patient has a pulmonary embolism, we need to categorize its severity. How do we do this?
Massive PE:
The clot is large enough that it is causing hemodynamic instability
This is a life threatening situation and requires immediate intervention from cardiac surgery or interventional cardiology
Submassive PE:
There is evidence of right heart strain but hemodynamic stability is maintained
You may see evidence of right heart dilation or bowing of the interventricular septum on TTE or there’s biochemical evidence of heart strain like an elevated troponin level or elevated BNP.
This may or may not require intervention like a thrombectomy or catheter-directed thrombolysis, and the interventional teams help make that call
Low-risk PE:
Everything else, and by far the largest category of PE.
These patients are generally treated with anticoagulation only.
The other way you’ve probably seen PE categorized is by anatomic location
Saddle PE extends across the bifurcation of the pulmonary artery
Segmental and subsegmental involve segmental and subsegmental branches of the pulmonary artery respectively.
How do we workup a patient in which we have a concern for a PE?
We can do a bedside TTE if we’re worried about massive/submassive PE, but if there’s less concern for that you can go right to CTA of the pulmonary artery to confirm the diagnosis of PE.
Formal TTE will be important during the patient’s admission as well to assess right heart function and pulmonary pressures.
For patients who are unable to get IV contrast for a CT scan, the VQ scan is available
This is a study with low spatial resolution
It can be helpful in the diagnosis of chronic PE, but in the acute setting, it will only pick out large-territory PE.
We also want to make sure we have CBC, CMP, and baseline coag labs all documented to help inform our anticoagulation plan.
If there is hemodynamic instability, how do we approach our patients?
First and foremost: Stabilization and restoring normal perfusion.
Since not all patients scream “PE” when they are being evaluated for shock, bedside echo can be invaluable here to give clues that acute right heart failure from obstructive shock is the driving pathophysiology.
We usually would manage this with empiric anticoagulation along with other critical care interventions like pressors, intubation, fluids, and even ECMO to try and maintain oxygen delivery to vital organs while a plan is made to intervene on the clot with either thrombectomy or catheter directed thrombolysis.
Often times, with this severity of illness, it won’t be possible to get CTA of the pulmonary arteries to fully define the clot burden, but if a patient can be stabilized after 15 min of resuscitation, they are generally able to have definitive imaging with CTA after that.
How do we approach diagnosis and management of deep vein thrombosis?
First establish if there is threatened limb perfusion
A large enough clot burden may dramatically impede blood return from the affected extremity that forward flow is impaired and the limb becomes ischemic
This is the so-called “phlegmasia” presentation - phlegmasia cerulea dolens and phlegmasia alba dolens
In this case, speak with IR or vascular surgery about a thrombectomy procedure to improve flow and restore adequate blood flow to the limb
If there is no concerns for limb compromise, get doppler ultrasound
Report will suggest if veins are “compressible.” If they are not, that suggest there’s something in the lumen, i.e., possibly a clot
The doppler portion will suggest if there is any blood flow.
One thing ultrasound isn’t always able to tell us is the age of a clot.
There are some features that suggest acute vs. chronic, but often comparison imaging is best for this.
Recall that a clot results in a pro-inflammatory environment.
The local inflammatory response may manifest as erythema over the area of the clot, and there can be intense pain associated with an acute DVT as well.
Patients can also have leukocytosis and fever because of this.
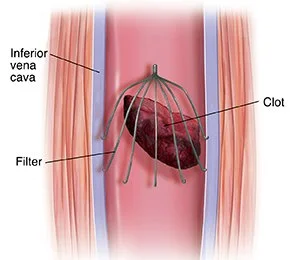
What is the role of an IVC filter in acute VTE?
An IVC filter works to catch large DVTs in the lower extremities, and in some cases, results in breaking them up into smaller clots, which may still get through the filter. (Think smaller PEs instead of a massive PE).
Image source: https://www.saintlukeskc.org/health-library/understanding-inferior-vena-cava-ivc-filter-placement.
No copyright infringement intended.
An IVC filter is a foreign material in the lumen of a vein, and therefore represents a potential nidus for thrombus formation.
Therefore, a filter is ONLY indicated if a patient has an absolute contraindication to anticoagulation and has a large lower extremity clot that represents high risk for embolization.
If an IVC filter is placed, ALWAYS have a plan to have it re-evaluated and removed
What do we need to know before starting patients on anticoagulation?
First: Determine symptoms and establish if this is provoked or unprovoked event
When he first noticed his leg swelling
If this was before or after onset of SOB
Was SOB onset insidious or sudden
Were there any provoking risk factors for VTE
If he’s ever had a VTE diagnosis before
If he’s ever had a serious bleeding problem like a GI bleed or brain bleed
Has he ever had any operations on his intestines, or any diagnoses of GI disorders that impairs his ability to absorb medications?
If there has ever been anyone else in his family with VTE diagnosis or history of other blood disorders
Understand bleeding risk
Use this to determine what anticoagulants are best and for the optimal duration of treatment
What are risk factors for VTE?
We can break provoking risk factors down into a couple of categories:
Major and minor
Transient and permanent
Major risk factors:
Major surgery
Pregnancy, recent delivery (within 6 weeks)
Exogenous estrogen exposure (HRT, OCPs, SERMs)
Traumatic orthopedic injuries
Metastatic cancer
Chemotherapy
Severe obesity
Paraplegia
Nephrotic syndrome
Inflammatory bowel disease
Other severe autoimmune disease
Hospitalization of 3 days or more
Although long flights and drives are what we always heard about in med school as risk factors for VTE, they’re actually considered minor provoking risk factors, along with
Minor surgery
Trauma without bone fractures
Hospital stay of less than 3 days
Being sick at home and immobile for 5 or more days
How do we determine duration of anticoagulation?
Largely based on if this is a provoked or unprovoked event:
For events provoked by a major transient risk factor, 3 months of anticoagulation is recommended (assuming the risk factor is no longer a factor)
For unprovoked events, indefinite anticoagulation is recommended
For patients with recurrent provoked VTE, or with VTE provoked by minor risk factors, the decision is a little bit less clear-cut, and you really have to talk through a patient’s risk tolerance, risk of bleeding, and tolerance of anticoagulation to figure out the best duration to recommend.
What is the mechanism of action of anticoagulants?
Goal of anticoagulation is twofold:
Prevent extension and embolization of the acute clot
Prevent additional thrombosis from developing elsewhere in the body
Once the clot is stabilized, the body’s own fibrinolytic system will work to digest away enough clot to restore blood flow.
If there is sufficient collateral flow or the body can increase the blood flow through collateral vessels, some residual clot may end up being there permanently, and is slowly transformed to a kind of scar tissue over time.
How do we select an anticoagulant?
Patient preference is paramount. Do not assume that a patient is opposed to injections (enoxaparin)
Some drug highlights (not all-encompassing)
Enoxaparin:
Pros: immediate onset with predictable levels, few drug interactions, approved in cancer-associated thrombosis
Cons: injections, cost, cannot be used in renal impairment
Warfarin:
Pros: Inexpensive, oral, the ability to monitor levels, easy to reverse (in emergencies)
Cons: Dietary/drug interactions, lab checks, increased risk of bleeding; inferior to enoxaparin in malignancy-associated VTE
DOACs:
Pros: Immediate onset, oral fewer dietary interactions, lower risk of bleeding compared to warfarin, non-inferior to enoxaparin for cancer-associated thrombosis
Cons: increased cost, need to be weary in patients with gastric surgeries, harder to reverse
Is there any monitoring that we need to do with DOACs?
In general, apixaban is safe for patients with normal liver function regardless of renal function, and dabigatran is safe for patients with normal renal function regardless of liver function.
There are no dietary restrictions for apixaban, and no requirement to be taken with food, unlike rivaroxaban, which requires a fatty meal for optimal absorption.
For patients on warfarin, it’s more important that if patients eat vitamin K-containing foods, that they try and eat the same amount week to week
This episode is sponsored by our Global Research Partners? Click here to get paid to participate in market research surveys!
The crew behind the magic:
Show outline: Daniel Hausrath
Production and hosts: Ronak Mistry, Vivek Patel, Dan Hausrath
Editing: Resonate Recordings
Shownotes: Ronak Mistry
Social media management: Ronak Mistry
We are proud to partner with HemOnc.org!
Want to learn more about the trials that lead to the regimens discussed today? What about dosing schedules? See links in the show notes for a link to HemOnc.org
Have some extra time and want to make some extra money? Click here to get paid to participate in market research surveys!