Episode 052: Breast Cancer Series, Pt. 1-Fundamentals of Diagnostic Radiology in Breast Cancer
The workup and management of breast cancer is complex! In this next series, we will dissect this topic inside and out. We will are so excited to be kicking off this series with special guest, Dr. Yasha Gupta to shed light on the role of our friendly breast radiologists and the very important role they/their team plays in the initial diagnosis and workup for a patient with a breast mass.
General reminders about breast cancer screening guidelines:
(Source: From our friends, The Curbsiders Episode 234 [https://thecurbsiders.com/curbsiders-podcast/234] ; No copyright infringement intended.)
Also be aware that special populations have slightly different guidelines. Refer to NCCN guidelines for details.
What is the difference between a Screening vs. Diagnostic mammogram?
Screening: no symptoms, no breast pain, no palpable lumps
Cranio-caudal view (CC) and medial lateral oblique (MLO) views
Bilateral
The addition of tomosynthesis
Diagnostic: patient has symptoms, patient is referred for abnormal exam, a lesion is seen on mammogram
If CC and MLO views
Spot compression views - additional compression/pressure on the breast to make mass more visible that is facilitated by positioning thanks to machine and technologist
Technologist play a very important role in this process
After the mammogram is completed, the patient is often waiting while the technologist discusses with radiologist about any further imaging that is needed
(Source: https://www.researchgate.net/publication/357776890/figure/fig3/AS:1111446595346444@1642000926845/Illustration-of-the-breast-view-angles-Craniocaudal-CC-Mediolateral-oblique-MLO.png ; No copyright infringement intended.)
(Created by Madeline Fitzpatrick, MD)
What is BI-RADS?
Stands for Breast Imaging Recording and Data System
This is how radiologists universally report and communicate breast imaging findings
Breakdown of BI-RADS scores:
0 = Incomplete, need to bring back for additional imaging
1 = Nothing visible on imaging that needs further follow up
2 = We see something, but it is benign (think something like a cyst)
3 = We see something, probably benign and has a <2% chance of malignancy
Lesions are to be followed with imaging every 6 months for at 2 years to ensure that the features continue to look benign
4 = Further workup is warranted, features suggestive malignancy
Often further broken down into A, B, and C (A = 5% risk of malignancy → C = 95% risk of malignancy)
5 = Suggest that lesion has >95% risk of malignancy, needs biopsy now!
6 = Biopsy-proven malignancy
TL;DR: Anything with BIRADS 4+ needs biopsy AKA anything with >2% chance of malignancy needs a biopsy
(Created by Madeline Fitzpatrick, MD)
If patient has BI-RADS 4+, is additional imaging needed?
At the discretion of physician/surgeon if they are looking for something else, but essentially a BI-RADS 4+ suggest that a biopsy is indicated at some point
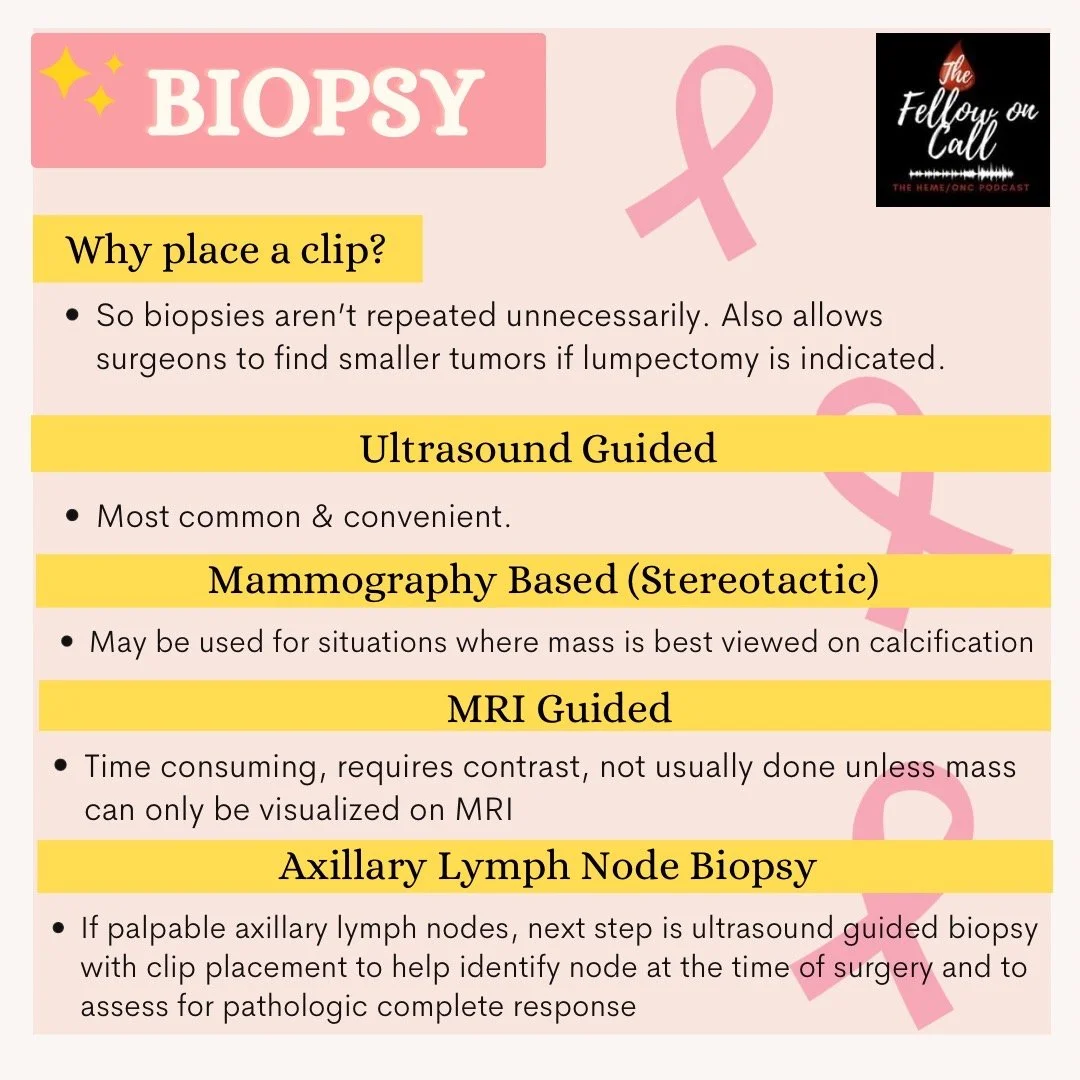
What are different techniques to perform the biopsy?
Ultrasound guided: Cheapest and fastest way to get biopsy done
Mammographically AKA stereotactic biopsies: Important for patients who have calcifications noted on imaging, which cannot be seen with ultrasound so they will need stereotactic biopsy
MRI: Last choice if the patient’s lesion can also be seen only on MRI.
These are more difficult to get simply because they take longer and fewer MRI slots available nationwide
More technically difficult, too
MRI has high sensitivity but lower specificity, therefore resulting in a lot of biopsies of lesions which may be benign (unnecessary workup being done)
If a patient has a lesion on screening mammogram that looks concerning for malignancy, is a follow up diagnostic mammogram required?
Diagnostic mammogram is to see it go away
If there is a definitive mass present, sometimes it is okay to skip the diagnostic mammogram and just go for ultrasound-guided biopsy, for instance
At the time of the biopsy, a marker will be placed so that on post-biopsy mammogram, we can localize the site that the biopsy was performed at
What is a marker clip?
This is a small piece of metal that is inserted at the site of the biopsy to mark where the lesion was
Why is this important?
When a patient gets a follow up mammogram in the future and a different radiologist reads it, they know that the area was previously biopsied
If it is malignant, can do “localization” where a radiofrequency or radioactive marker can be placed so surgeon knows where to do the surgery
What if the patient had BI-RADS 0 (incomplete picture) on screening mammogram, what happens next?
If patient has a mass on mammogram with focal asymmetry: They come back from mammogram and ultrasound
If calcification is noted: They return for “magnification views” so that we can better classify them
MRI only used when there is no other option, for instance if the mass is only seen on “contrast enhanced mammogram”; MRIs are very sensitive, which means we may sample more than is necessary
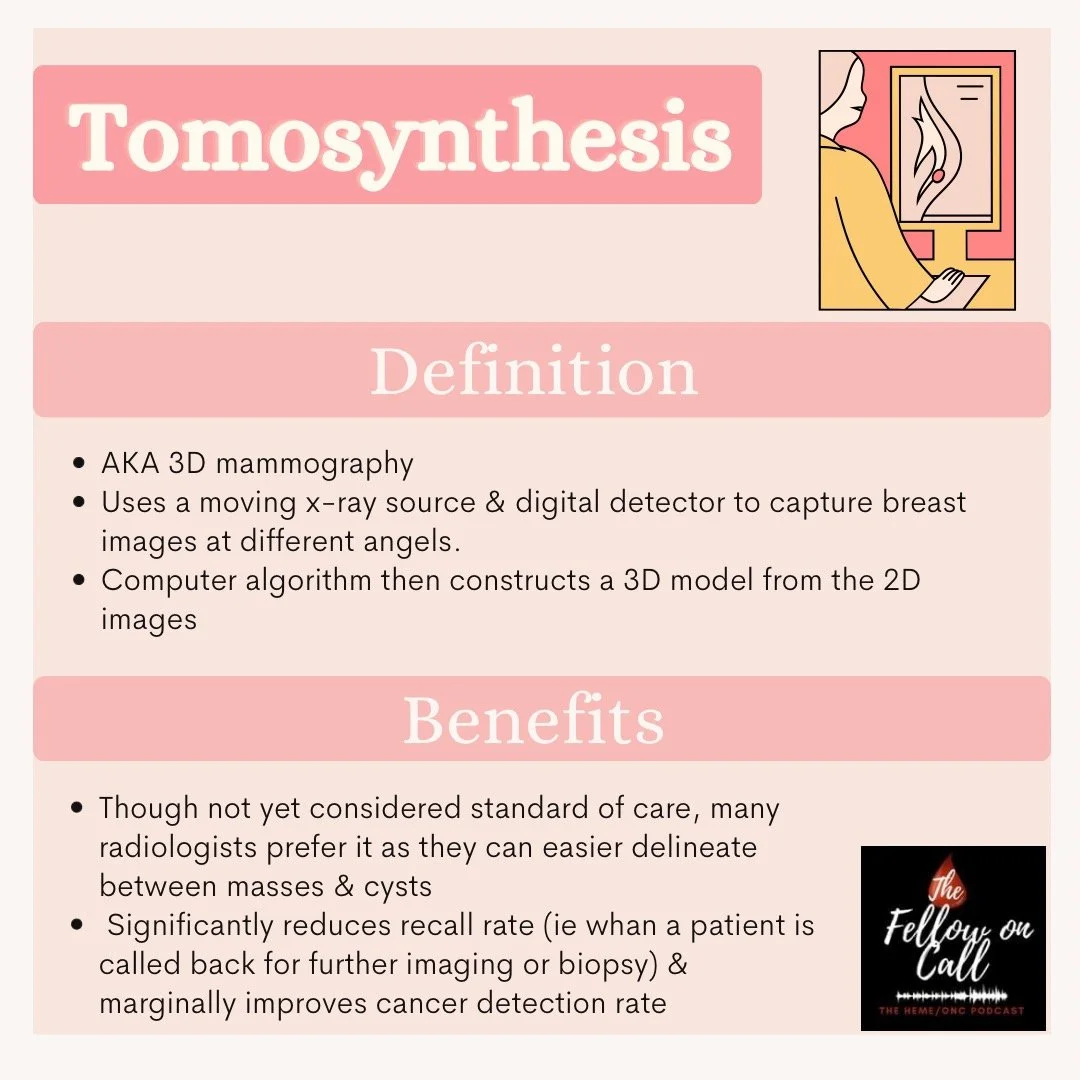
What is tomosynthesis?
This is a 3D view of the breast
Allows for better characterization of abnormalities seen on imaging
Makes architectural distortion easier to characterize
Improves re-call rate, i.e., calling patient back for repeat imaging
There was a study by the PROSPR consortium that showed tomosynthesis combined with digital mammography had improved invasive cancer detection rates from 3 per 1000 to 4 per 1000, suggesting this may not be cost effective for a marginal benefit and the harm of over biopsy.
Yasha reminds us that although the data suggests only a small increase, that could make a big difference in outcomes for that 1 patient who does have positive findings on tomosynthesis not seen on 2D view, therefore she favors using this approach
(Created by Madeline Fitzpatrick, MD)
What type of biopsy is best?
Always advocate for core! More tissue allows better characterization and for additional ancillary testing
When we have palpable lymph node, what is the process of getting a biopsy? If we got an MRI for evaluation, does the MRI characterize axillary findings?
If there is concern for axillary lymphadenopathy, use ultrasound to check axilla.
Radiologist is looking for lymph node cortical thickness >2mm and changes in shape (reniform to round)
Mammogram is not used to assess axillary lymph nodes
MRIs always get the axillary lymph nodes, as well as internal mammary chain; but often ultrasound is still performed after MRI
What if someone doesn’t have palpable lymph nodes? Is imaging indicated?
This is based on the institution and based on local practices of surgeons
When axillary lymph node is biopsied, is a marker clip placed, as well?
Also institution-specific
(Created by Madeline Fitzpatrick, MD)
About our Guest:
A huge thank you to Dr. Yasha Gupta (@yashaguptamd) for joining us for this awesome episode. Dr. Gupta completed medical school at Central Michigan University College of Medicine. She completed her residency at Mount Auburn Hospital in Cambridge, Massachusetts. She is completing her Breast Imaging fellowship at Memorial Sloan Kettering in New York City. In addition to being a radiology fellow, she is Chair of The American College of Radiology (ACR) Resident, Fellow and Student (RFS) Section, is active on YouTube, and a new mom!
The crew behind the magic:
Show outline: Vivek Patel
Production and hosts: Ronak Mistry, Vivek Patel
Editing: Resonate Recordings
Shownotes: Ronak Mistry
Infographics: Madeline Fitzpatrick
Graphics, social media management: Ronak Mistry