Episode 051: Heme Consults Series- Approach to Inpatient Leukocytosis
We are kicking off our intermittent “Heme Consults Series” with a great overview of the approach to leukocytosis, a common question we get on the wards. In this episode, we talk about the initial steps we should take to triage these cases and what we should be thinking about in regards to next steps.
Also - a huge shoutout to one of our listeners who had emailed us and said this is a common question that puzzles them in their work as a hospitalist! If there is something that you’d like to hear us cover in this series, definitely reach out!
This is a very broad topic, so the goal here is to give an initial road map of where to go next.
Background
Only a small fraction of our total body WBCs is measured on the CBC
At any given time, most of our WBCs are either in the bone marrow or “marginated” (i.e., stuck to the vessel walls)
At the time of an insult, there can be a rapid rise in the white blood cells circulating as these cells are demarginated
Most of these cells are neutrophils
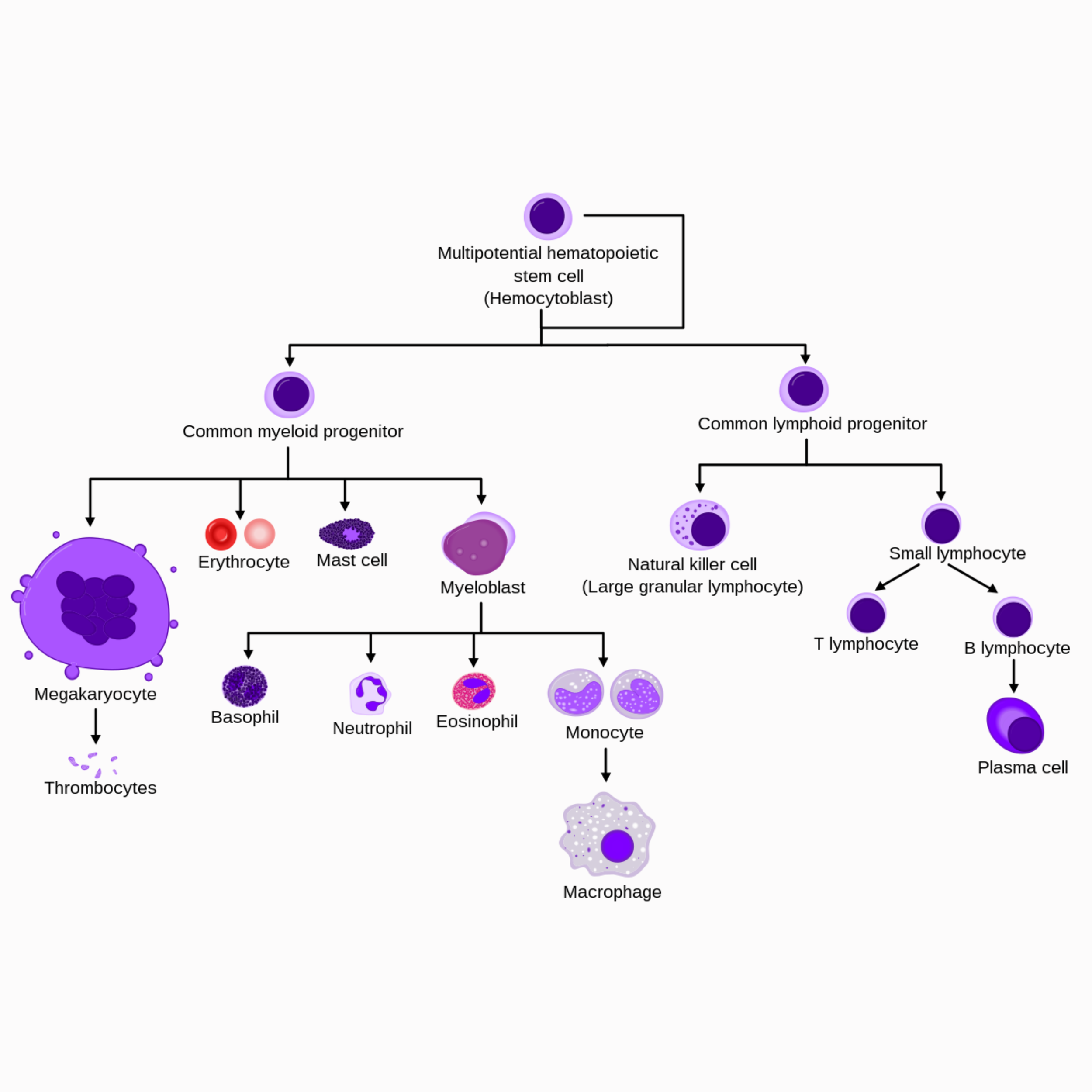
(Source: https://upload.wikimedia.org/wikipedia/commons/thumb/f/f0/Hematopoiesis_simple.svg/1280px-Hematopoiesis_simple.svg.png ; No copyright infringement intended.)
Leukocytosis Workup:
History:
Chronicity
Context
Constitutional symptoms
Medical history (chronic inflammatory states)
Medications (growth factor, steroids, lithium, OTC meds)
Social history (smoking, obesity)
Surgical history (splenectomy)
Family history
Physical
Lymphadenopathy, splenomegaly, rashes
Initial lab evaluation:
Repeat CBC
Peripheral smear (abnormal cells, platelet clumps, blasts, hemolysis?)
Manual diff
Where to go next is dependent on the primary cell type(s) noted on the manual diff that are contributing to the leukocytosis!
Neutrophilia:
Most common subset of leukocytosis
Usually, a leukemoid reaction from illness
No constitutional symptoms or abnormal cells on smear 🡪 consider observation
If secondary causes have been ruled out and there is a left shift, this may suggest the presence of malignancy, such as CML or myeloproliferative neoplasm (PV and myelofibrosis). May need bone marrow biopsy or testing for BCR-ABL, JAK2, CALR, MPL.
Eosinophilia:
Hypereosinophilia: > 1500 eos/microL
Hypereosinophilic Syndrome: > 1500 eos/microL (on two occasions >/=1 month apart) + end organ damage
If a patient presents with HES, additional workup is warranted. Workup includes the PDGRA fusion gene (for myeloproliferative neoplasm), BCR-ABL (for CML), JACK2 V617F mutation, bone marrow bx.
Hydroxyurea can be used to treat HES with end organ damage and won’t compromise future diagnostic testing
Basophilia:
If >10-15% predominance, this raises concern for CML
Monocytosis:
Once you rule out infections, consider myeloproliferative neoplasm
Lymphocytosis:
Assume viral infection until proven otherwise
Rarely, can be caused by a clonal process like CLL (lymphocyte count > 5000)
References:
https://www.nejm.org/doi/full/10.1056/nejmoa025217: article about PDGFRA and FIP1L1 Genes playing a role in hypereosinophilic syndrome
https://www.haematologica.org/article/view/5345: article about T-cell abnormalities in hypereosinophilic syndrome
https://www.uptodate.com/contents/approach-to-the-patient-with-neutrophilia?search=neutrophilia%20§ionRank=2&usage_type=default&anchor=H9379019&source=machineLearning&selectedTitle=1~150&display_rank=1#H835275612: approach to neutrophilia
https://www.uptodate.com/contents/hypereosinophilic-syndromes-clinical-manifestations-pathophysiology-and-diagnosis?search=fip1l1%20pdgfra&source=search_result&selectedTitle=1~51&usage_type=default&display_rank=1: approach to hypereosinophilic syndrome
https://www.uptodate.com/contents/approach-to-the-adult-with-lymphocytosis-or-lymphocytopenia?search=lymphocytosis&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H1516036561: approach to lymphocytosis
Hematology and Oncology subspecialty consult, WashU St. Louis
The crew behind the magic:
Show outline: Ronak Mistry
Production and hosts: Ronak Mistry, Vivek Patel, Dan Hausrath
Editing: Resonate Recordings
Shownotes: Madeline Fitzpatrick, Ronak Mistry
Graphics, social media management: Ronak Mistry