Episode 091: Heme Consult Series: Intro to Acquired Hemolytic Anemia and G6PD Deficiency
It’s time for another heme consult series, this time focusing on hemolytic anemias. In this multi-part series, we will go through our approach to thinking about concerns for hemolytic anemias. This is super high yield for anyone who cares for patients, especially those in hematology/oncology. It’s not uncommon to get a consult on the heme consult service for assistance with diagnosis and management of suspected hemolytic anemias!
What is “hemolytic anemia?” When should we suspect it?
Breakdown of RBC due to an intrinsic or extrinsic failure of RBC function or structure
Consider hemolytic anemia in your differential diagnosis when patients present with unexplained anemia, remembering that the most common cause of anemia is going to be bleeding!
Key questions to ask your patients in the history:
Onset / Associated Symptoms: Fatigue, jaundice, abdominal pain, scleral icterus, abdominal pain, dark urine
Chronicity / Recurrence
Recent Illness
“B-Symptoms”
Family History / Personal History: RBC Disorders? Early Gallstone Disease?
Recent Surgeries?
Recent Blood Transfusion
Indwelling / Support Devices: Prosthetic Valves, Extracorporeal Cardiopulmonary Support (ECMO) Cannulas / Circuit
Key components of the physical exam:
Jaundice
Scleral icterus
Splenomegaly
Dark Urine
If there is a suspicion for hemolytic anemia, what is the workup?
Peripheral smear: paying attention to morphology of cells
Repeat CBC: important to look at hemoglobin, MCHC, MCV, and RDW
Reticulocyte Count (Retic Count)
CMP: Particularly the indirect bilirubin
LDH
Haptoglobin
Direct antiglobulin test (DAT)
What is the “DAT”?
Also referred to as the Coombs test; it is an assay testing for antibody binding to RBCs leading to hemolysis
DAT Caveats:
7 – 8% false positive hospitalized patients without clinical evidence hemolysis
Will NOT detect low levels of IgG or complement
MISSES IgA and IgG4 antibodies
How the test is performed:
RBCs washed to remove any unbound antibodies/complement
Mixed with anti-IgG and anti-C3 antibodies
If either IgG or C3 is present on the RBC surface, this leads to agglutination = positive test
An elution screen is also performed, which is the process by which the pathogenic antibodies are extracted off the RBCs and then they’re tested against RBCs with known antigens
It’s like a Sudoku puzzle! Trying to see what pattern of antigen expression causes agglutination. This allows you to determine what epitope the antibodies causing hemolysis are directed against.
If DAT+ but elution is negative, it brings to question if the antibodies that were detected on the DAT are truly pathogenic, noting again that many patients can have a positive DAT without clinical evidence of hemolysis
If the DAT is negative, there are additional things you can do like a “super Coombs,” but in MOST cases, a negative DAT will argue against an acquired hemolytic anemia
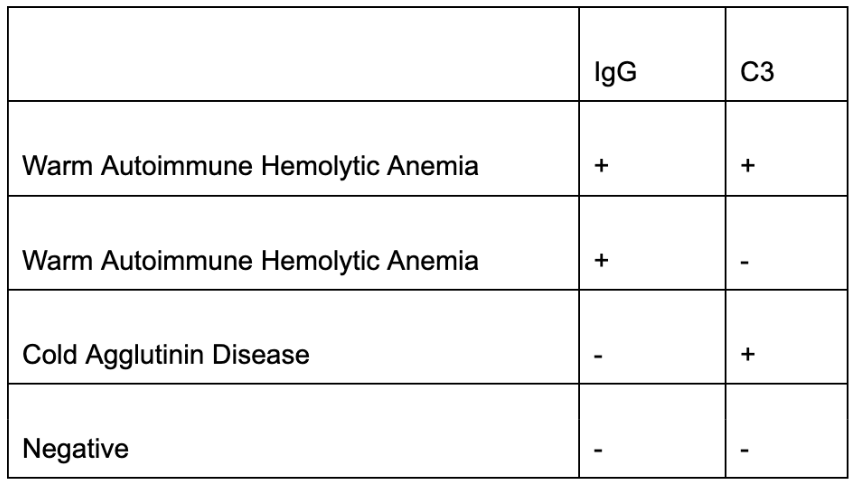
Possible outcomes from DAT test and corresponding diagnoses to consider; Chart created by Ronak Mistry
In some cases, patients may have congenital causes of hemolytic anemia. One of the most common causes of congenital hemolytic anemia is G6PD deficiency.
In the overall population, this is rare, however still the most “common” enzyme deficiency causing hemolytic anemia.
1 per 20,0000 Caucasians
More common in people of Middle Eastern and African-American descent
Pathophysiology
X-Linked Mutation (therefore more common in males.
There are over 400 different mutations!
When to suspect G6PD deficiency: concerns for hemolysis, often after new medications are started (or classic board question - when someone consumes “fava beans”) or even acute stress
Can also think about genetic testing if suspecting G6PD deficiency
Treatment: Supportive care in the acute setting
Important caveat about testing:
Not easy to test acutely after hemolysis occurs because the cells to diagnose this, we test “G6PD levels” which are activity levels. In an acute crisis, the cells with the abnormal G6PD enzymes will have already hemolyzed so levels can appear falsely normal
Long list of drugs to check if patient is on when suspecting G6PD deficiency
References:
Wintrobe’s Hematology, 14th Edition
The crew behind the magic:
Show outline: Ronak Mistry
Production and hosts: Ronak Mistry, Vivek Patel, Dan Hausrath
Editing: Resonate Recordings
Shownotes: Zach Wills, Agrima Mian, Ronak Mistry
Social media management: Ronak Mistry
We are proud to partner with HemOnc.org!
Want to learn more about the trials that lead to the regimens discussed today? What about dosing schedules? See links in the show notes for a link to HemOnc.org